The idea of nurses and smoking may feel contentious and probably does not ‘fit’ in many people's minds. It is well known that smoking carries serious health risks – the evidence is clear that smoking causes and contributes long-term illness. Therefore, a healthcare professional smoking may seem counterintuitive; yet many do.
Of course, this does not only affect nurses. Tobacco dependence among NHS staff in general remains an important issue. Tackling smoking is a key component of the NHS Long-Term Plan and forms the NHS's contribution to the government's wider 2030 smoke-free ambition (NHS, 2019; Department of Health and Social Care (DHSC), 2023).
There is evidence that support from nurses can help people to stop smoking (Rice et al, 2017), which suggests that nurses can exert a positive impact on poor health related to tobacco, including chronic respiratory disease. But can nurses who smoke have the same impact? There is some evidence indicating that nurses who smoke feel less confident in their ability to help people quit (Slater et al, 2006).
Smoking rates in the UK have been steadily falling and are now estimated to be down to 11.9% of the population (ASH, 2024). However, there is a greater prevalence of smoking in some groups, such as among those with mental health challenges, and tobacco dependence remains a key contributor to ill health. One may assume that nurses are less likely to smoke than the general population, given their overall health knowledge and health literacy levels. However, it is well known that stress can be a trigger for many to smoke, including ex-smokers and those trying to quit.
The authors wanted to explore the scale of this issue, including the reasons why nurses smoke when they understand the harmful effects on their health, as well as the support that could be offered to help nurses to quit smoking.
Project aims and partners
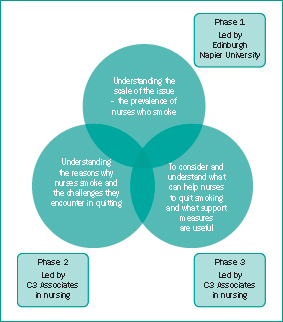
There were three key aims of this project:
The project received funding from the Burdett Trust for Nursing's chronic respiratory diseases programme. It was a joint initiative between three partner organisations:
‘In a matched analysis based on age, sex, economic activity and socioeconomic group, there was little difference in current smoking prevalence between nurses and those who were not nurses.’
Project overview
The project took place between January and December 2024. It was set up in three phases, with each phase informing the next (Figure 1). Table 1 shows the various project activities undertaken during each phase.
| Phase | Aim | Project actions |
|---|---|---|
| Phase 1 | Understand the scale of the issue (the prevalence of nurses who smoke) | Analysis of smoking in nurses, based on annual population survey data |
| Phase 2 | Understand the reasons why nurse smoke and the challenges they face in quitting | Online survey to identify nurses who smoke or used to smoke. Recruitment of nurses who smoke or are ex-smokers to explore their reasons for smoking and perceived barriers to smoking cessation. Data collected through an online focus group and 10 semi-structured interviews |
| Phase 3 | Consider and understand what can help nurses to quit smoking and what support measures are useful | Provide participating nurses with access to free resources to support them with smoking cessation, including the Smoke Free app and a digital toolkit |
The Smoke Free app was a key part of the support provided to participating nurses. The app is a fully digital service that provides 24/7 live support from trained advisors. It has many automated features, such as progress indicators that show the length of time the user has been smoke free, the number of cigarettes not smoked, the health benefits as they accrue, and the money saved. Project participants were also offered nicotine replacement therapy and vapes, as the Smoke Free app team advised that this is often helpful. As the app is not set up for more robust health assessments, other medications were not offered as part of this project, but the advisors would recommend that the participant visit their GP if any issues arose.
The project was presented at a learning and wellbeing event at the 2024 Royal College of Nursing congress to promote the work with key stakeholders. An online webinar event was also held via the Learn With Nurses online platform to discuss the findings of the project. Various additional engagement activities were carried out via social media platforms, including Facebook, LinkedIn and X, to promote the work and raise awareness of the Smoke Free app.
Insights gained from across the three phases helped to inform the co-production of a digital toolkit known as ‘Nurses and smoking – a breath of fresh air’, which is available online (C3 Collaborating for Health, 2024). This provides ongoing support for nurses to help both themselves and their patients to reduce the risk of chronic respiratory disease.
Challenges
Attracting participants for the project was the biggest challenge. In previous projects, C3 Collaborating for Health had used social media to recruit participants for surveys and projects, alongside other incentives. For this work, a shopping voucher was given to all participants, as well as access to the Smoke Free app and nicotine replacement options.
However, using social media caused difficulties, and some links were used to direct multiple people to the inclusion survey, generating thousands of bogus responses. Exactly why this happened is unknown, but the authors believe that people were trying to access the vouchers. To overcome this challenge, separate links were used, so they could be separately switched off quickly and posted only on closed nursing networks. X (formerly Twitter) was avoided, to increase control over access. The IP addresses from scam responses were checked to see if any could be genuine, and any email address with a unique IP address was contacted, but all were found to be false, so the authors feel confident that no interested nurse had been missed. However, this did mean that far fewer nurses took part than initially envisaged.
Summary of findings
From the 3-year survey dataset (spanning January 2020 to December 2022), 3123 nurses were identified. Younger nurses (20–29 years old) were found to have a slightly higher current smoking prevalence (8.4%) than nurses aged over 30 years (5.2–6.2%). In a matched analysis based on age, sex, economic activity and socioeconomic group, there was little difference in current smoking prevalence between nurses and those who were not nurses (6.0% vs 5.9%).
‘Being a smoker affected the way participants interacted with their patients. Many of the focus group attendees said that they did not discuss smoking with patients and did not feel able to advise on stopping smoking.’
The survey, interviews and focus group comprised a relatively small number of participants: the survey had 18 responses, 10 participants were interviewed and the focus group had 14 attendees. Of these 42 individuals, 26 took up the option to use the Smoke Free app. Nine of these 26 individuals requested nicotine replacement products, all of whom stopped smoking.
The wider feedback from app users was positive, with focus group participants describing how valuable they had found the app and the support it provided, stating that this had contributed significantly to their ability to quit smoking. They particularly liked the convenience of the app, with one participant saying it was like having ‘an advisor in your pocket’.
Nurses in the focus group generally agreed that changing shift patterns made committing to attendance at a stop-smoking clinic difficult, but that being able to speak to an advisor at any time of the day or night via the app suited their working lives. They were also appreciative of the free vape they received alongside the behavioural support, and the reassurance that switching to vaping was a popular and effective way to stop smoking.
The small number of nurses involved is an obvious limitation of the project. However, all participants gave similar reasons for why nurses smoke and the barriers to quitting, so the project team feel confident that these results are representative. Participants included nurses working in community, primary and secondary care and at a range levels, such as registered nurses, nursing associates and students. Four key themes were identified in the analysis, as presented in Table 2, with further analysis in Figure 2. Overall, there were some perceived benefits of smoking described by nurses; most notably, that smoking increased the likelihood of them getting a break from work and providing opportunities to socialise. The participants were aware of the health consequences of smoking. However, although this was considered to be a driver to stop smoking, many did not feel an immediate need to stop, as long as they felt well and saw themselves as healthy. Several nurses cited the impact on family and dependents as a reason to stop smoking.
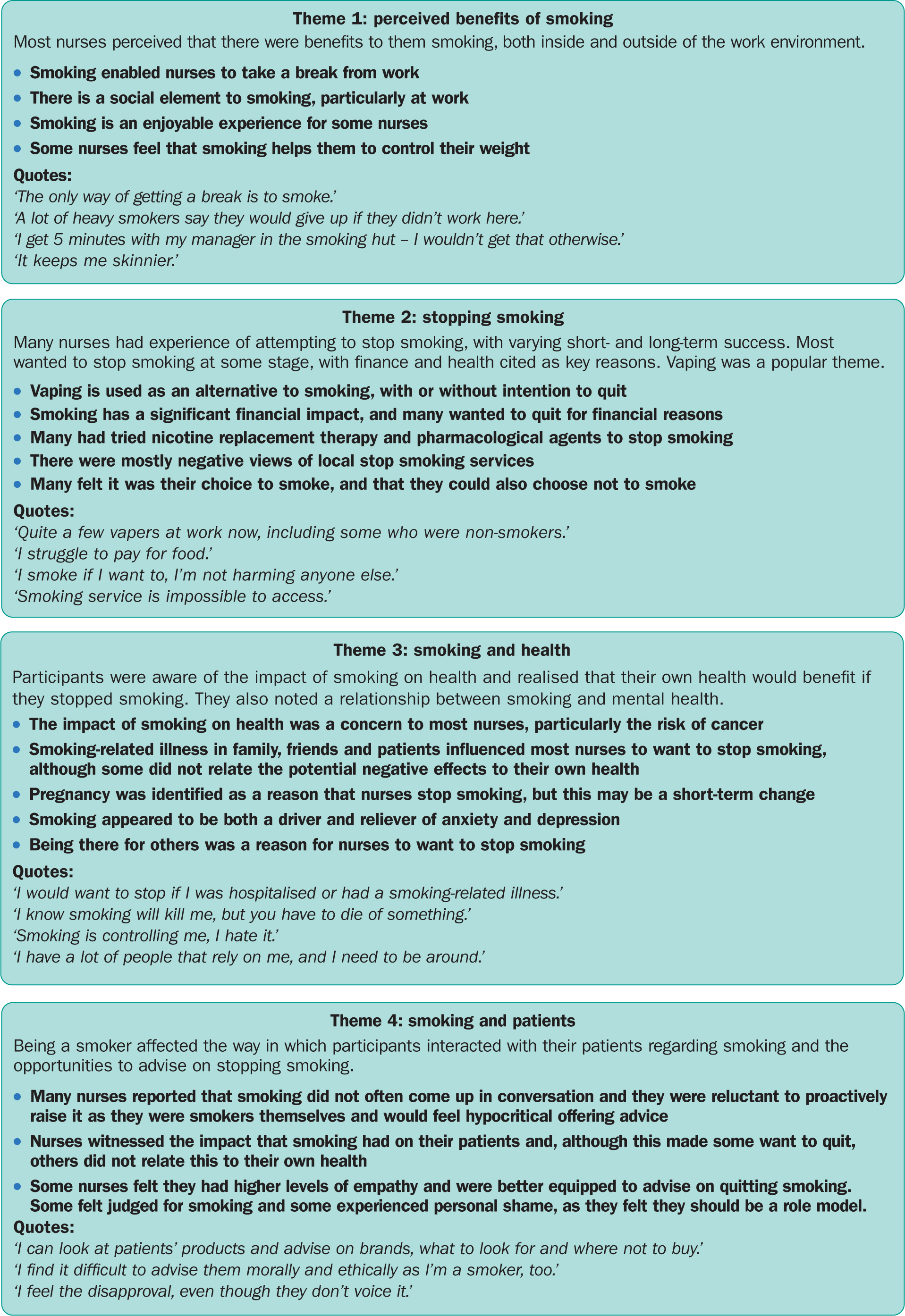
Being a smoker affected the way in which participants interacted with their patients. Many of the focus group attendees said they did not discuss smoking with patients and did not feel able to advise on stopping smoking. Conversely, some felt that being a smoker enabled them to build rapport and feel higher levels of empathy for patients who smoke.
Recommendations
It is widely acknowledged that, while nursing can be rewarding, it is a challenging profession. Nurses are often under considerable stress, and balancing high workloads with inadequate staffing and skill mixes is an ever-present challenge (Daniel et al, 2024).
Previous analysis has identified stress and frustration among nurses, many of whom report being unable to do their jobs adequately, which is a major reason for nurses leaving the profession (Leary et al, 2024). One of the key themes identified in this project echoes this wider work on the complexity and challenges of nursing. Some of the reasons given for why nurses smoke, such as to have an excuse to take a break, or get 5 minutes with their manager, suggest that these are not otherwise easy for them to do.
It is beyond the scope of this article to detail the steps that healthcare organisations need to do to prevent nurses from leaving the profession. Improving nurse retention is multifaceted and has been widely reported (Greenley et al, 2024). However, it is clear that systems and organisations need to do more to support staff wellbeing generally, such as ensuring that they are able to take their breaks and have line manager support, particularly for those wanting to stop smoking. Tobacco dependence among NHS staff is an important issue. Helping to tackle it is integral to wider aims for a smoke-free society, and nurses helping people to quit is essential to achieving this goal (Waterall and Fisher, 2024).
It is essential for nurses to know how to have conversations with patients and service users about stopping smoking, whether or not they smoke themselves. The National Centre for Smoking Cessation and Training (www.ncsct.co.uk) offers free online training designed to support this, giving information on how to raise the subject of smoking and provide advice and some brief interventions.
This project identified that nurses who smoke know that it can hinder their willingness to help their patients stop smoking. The analysis also showed that many had tried to quit smoking numerous times in the past, emphasising the need for support. This should be made available to staff through resources such as the Smoke Free app, as well as nicotine replacement products. There is evidence that using support and effective quitting aids leads to greater success than trying to quit alone (Jackson et al, 2025).
Conclusions
This project was relatively short, spanning just 1 year, and as such the evidence from it is limited. However, the findings do reflect themes relating to the challenges that nurses face to quit smoking, which are similar to those seen in the general population. The themes also reflect some of the wider difficulties that nurses experience in managing their wellbeing, and a need to support nurses more generally with their health.
As part of this, it seems essential to give greater focus to smoking cessation support for nurses and other healthcare professionals. It should not be assumed that, just because they know that smoking is bad for them and even see the effects with their patients, nurses themselves will be able to stop without help. Access to support from employers and line managers is essential, as well as providing ongoing professional development to ensure that nurses have up-to-date information and resources on how to support themselves and their patients.

