There is a long history of nurses in general practice having poorly coordinated access to education and variable employment conditions (Atkin and Lunt, 1993; Crossman, 2008; Queen's Nursing Institute [QNI], 2016). The flexibility of their employment model in general practice has attractions but also a down-side, as it limits their ability to negotiate minimum standards of professional development support if they are lacking. These forces in combination affect general practice nurses' (GPNs') perceived level of empowerment and influence at a time they most need to step-up their game to cover the demands in general practice, particularly post-COVID-19. There is a recruitment and retention crisis impacting on GP practices across the UK (Napier and Clinch, 2019). The GPN workforce is fairly stable but predominantly populated by those over 45 years old. The increasing pressure in general practice and the current changes in the structure of primary care puts GPNs in the spotlight as they help their GP colleagues to try and maintain excellent primary care. Finding time to devote to maintaining their continuous professional development and understanding the complex matrix of education on offer is therefore a real challenge, which poses a risk to ensuring quality of care and patient safety.
Capital Nurse
Capital Nurse is a time limited initiative for all nurses in London, running from 2015 until 2020 funded by Health Education England (HEE), NHS England (NHSE) and NHS Improvement. The Capital Nurse vision is to ‘get nursing right for London’, ensuring that London has the right number of nurses, with the right skills, in the right place, working to deliver excellent nursing wherever it is needed (Capital Nurse, 2018). There are two pan-London workstreams: ‘Routes into nursing’ and ‘Retention’. The retention workstream has 3 sub-groups—‘preceptorship’, ‘career framework’ and ‘Qualification in Specialism’ (QIS). The QIS programme has created several career development support tools and accredited qualifications, mainly in urgent and critical care. Since 2018, the work has focused more on GPNs, with approval of a two-phase project to develop a QIS standard for junior GPNs which commenced in early 2019.
Rationale for the project
Due to the independent business model of general practice, GPN recruitment and retention is often inconsistently managed and development opportunities can seem invisible to GPNs (Royal College of General Practitioners [RCGP], 2013). Some practices may be very proactive in workforce planning and team development, others may recruit only when nurses are leaving. In addition, applicants for vacancies may come from a wide range of clinical settings, often with little or no primary care experience, resulting in a skills gap for working in general practice, particularly if they are newly qualified. As the role of the GPN often involves working autonomously, sometimes geographically and professionally isolated, it can be a challenge to develop new skills while in the job and there are many examples of ad hoc training of varying quality to meet the priority needs of the practice. This inevitably leads to variability in standards of education and levels of competence in junior GPNs. This project seeks to address this inconsistency across London by creating a standard for GPN education, to secure a sustainable, consistently trained GPN workforce for the future. This standard will have relevant application across a wide range of partners involved in supporting GPNs to develop the skills they require (Figure 1).
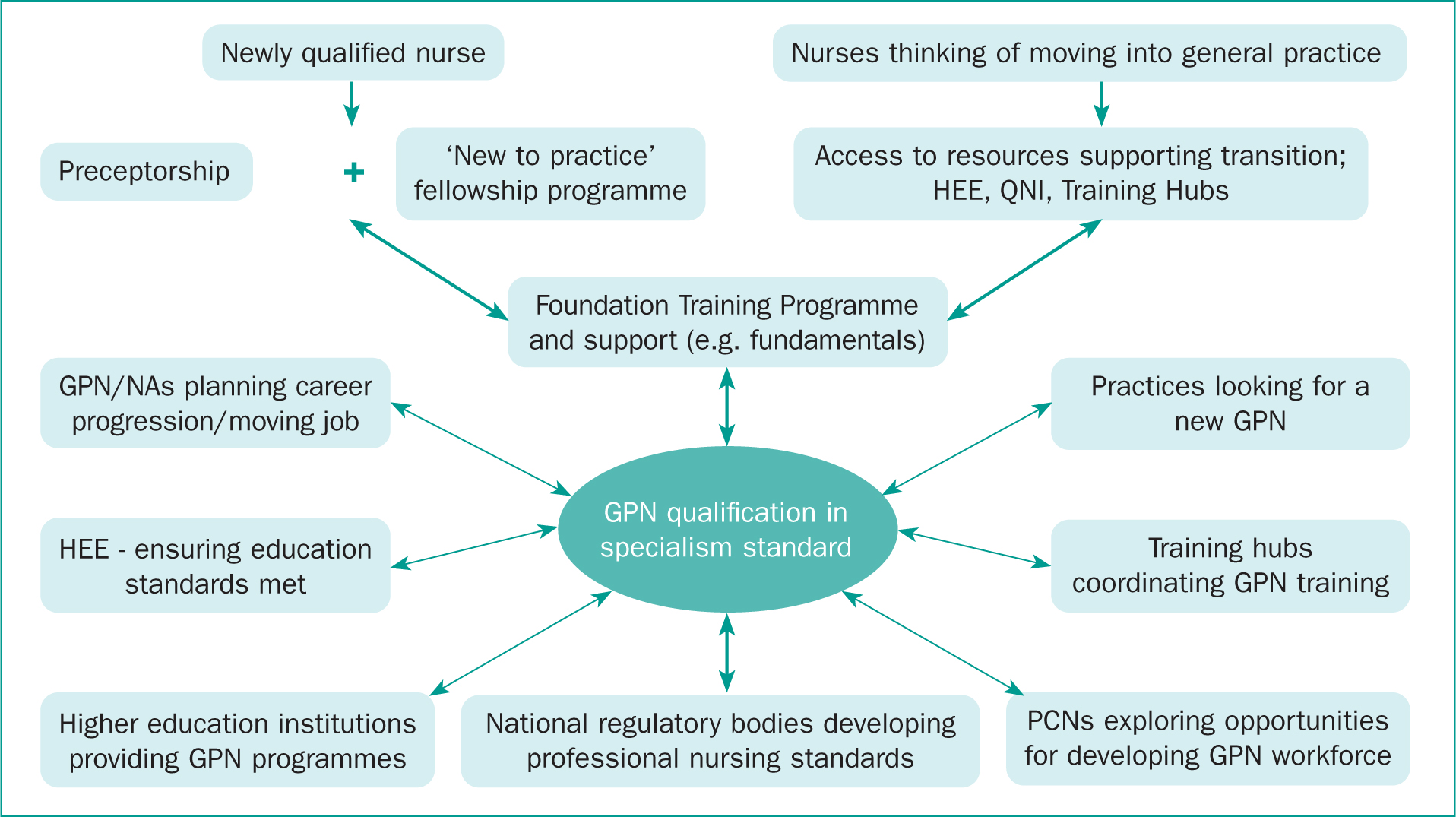 Figure 1. Who will use the Capital Nurse general practice nurse (GPN) Qualification in Specialism Standard (QISS): minimum requirements for professional development programmes for new GPNs. HEE, Health Education England; NA, nursing associate; PCN, primary care network; Queen's Nursing Institute.
Figure 1. Who will use the Capital Nurse general practice nurse (GPN) Qualification in Specialism Standard (QISS): minimum requirements for professional development programmes for new GPNs. HEE, Health Education England; NA, nursing associate; PCN, primary care network; Queen's Nursing Institute.
Policy context
A key feature of the NHS Strategic Plan—the ‘5 Year Forward View’ (5YFV) (NHSE, 2014) and subsequently the ‘Long Term Plan’ (NHSE, 2019)—was to strengthen primary care as it is well recognised that this initial point of contact with the public is the critical place for effective early intervention to maintain optimum health and wellbeing and to reduce the pressure on hospital services and social care. The new care models set out in the 5YFV encouraged collaborative primary, community and secondary care provision and shared expertise and resources to improve patient outcomes. The government developed a specific plan for general practice, the ‘GP Forward View’ (GPFV), with the aim to reinvent the clinical model, career model and business model at the heart of general practice (NHSE, 2016). In the GPFV the government sets out 5 priorities to underpin this process, with funding to support the programme:
- Investment
- Workforce
- Infrastructure
- Workload
- Care re-design.
With a focus on the programme tackling workforce challenges, NHSE developed a specific plan for nursing, the GPN 10 Point Plan (NHSE, 2017), which sets out a series of goals for partner organisations involved in recruiting and developing GPNs for the future workforce. A wide-ranging programme of work was funded under this plan, each of which is designed to achieve one of the 10 goals. This project is particularly relevant to Goal 7: ‘Support access to educational programmes’.
Developing the prototype
Capital Nurse approved the initiation of the project to design a Qualification in Specialism Standard (QISS) for GPNs, using a model already developed and implemented in several areas of acute nursing (emergency care and neonatal care). However, it quickly became apparent that the existing model addressed a very different branch of nursing, where consistent employment conditions, job descriptions and mandatory training requirements were well established. This could not be further from the case in general practice. For this reason, the GPN QISS became focused on developing a standard that would guide such consistency, to address the wide variation which exists. The key tasks for Phase 1 of the project are illustrated in Table 1.
Table 1. Qualification in Specialism Standard (QISS) Phase 1: key tasks
| Review of literature, relevant policy, existing frameworks and programmes of education |
| Cross comparison of key general practice nurse (GPN) standards and frameworks against Capital Nurse Qualification in Specialism (QIS) structure |
| Synthesis of an outline structure for GPN QISS Stakeholder input to critique, ensure relevance and value for GPNs, co-design the standard |
| Stakeholder input to critique, ensure relevance and value for GPNs, co-design the standard |
| Report to Capital Nurse steering group |
‘It is vital that GPNs are properly supported and developed in order to maintain a high standard of first-contact care in general practice.’
Matrix analysis
In order to adopt a collaborative, inclusive approach and ensure the prototype GPN QISS included the best of everything already developed, a comprehensive review and cross-comparison of the key components of existing national frameworks and standards was conducted. The outcome of this analysis was then synthesised into a prototype for co-development, using the generic headings of the existing Capital Nurse QIS.
The prototype identified the following eight standards for development:
- A curriculum overarching standard, with aim and outcomes
- Common core curriculum elements—minimum consistent programme content
- Specified essential skills and competencies, clinical domains, HEE framework level
- Blend of academic and practical components
- Assessment processes and academic credits
- Quality monitoring procedures
- Networking and support resources for continuing professional development (CPD) and career progression
- Specific responsibilities for education providers, learners, employers and supervisors/assessors.
A discussion paper with draft content for the standards was shared with a wide group of stakeholders, inviting them to contribute to co-designing them.
Co-design with stakeholders
There was a good response to the initial invitation and a stakeholder meeting was held to discuss the relevance of the GPN QISS and the appropriateness of the draft content in the standards, with representation from across the London system as illustrated in Table 2.
Table 2. Stakeholder involvement in co-design
| Sustainability and transformation partnerships (STPs) | Queen's Nursing Institute (QNI) |
| Clinical Commissioning Groups (CCGs) | Royal College of Nursing (RCN) |
| Training hubs Local Medical Committee (LMC) | Health Education England (HEE) GP federations |
| Universities | NHS England |
| Capital Nurse | GPN educators |
There was a consensus from the group that it would be useful to develop the prototype further and to extend the stakeholder group to include primary care networks (PCNs) and GPN educators. A workshop was arranged with every attendee having the opportunity to scrutinise and comment on the content in each of the 8 standards. The outcomes from this stakeholder workshop were incorporated into the QISS, which was subsequently approved by the Capital Nurse board for testing in practice with training hubs and education providers.
Testing the QISS in practice
The goal of GPN QISS is to promote a standardised approach across all education providers in terms of the courses they offer to junior GPNs. Meeting the requirements of all 8 standards would achieve ‘QISS compliance’, giving the provider a kite-mark that would be recognised as a consistent standard across different sites and practice settings.
Education programmes available
In 2018, HEE commissioned a harmonised, pan-London training for new GPNs with funding allocated through local community education provider networks (CEPNs)— now transitioned to become training hubs—and a tri-partite recruitment process between the GP employer, training hub and higher education institution (HEI) running the programme (HEE London, 2018). There are two academic levels of accredited programme on offer, provided by 7 HEIs across London, with both levels requiring the employing practice to sign a contract with the training hub regarding the terms and conditions of the training. In addition to these HEI programmes, there are other resources supporting nurses new to general practice which are not funded through HEE and are more variable in terms of content and outcomes. These include online resources such as the QNI ‘Transition to General Practice Nursing’ (QNI, 2019) and the London-wide local medical committee (LMC) ‘General Practice Nursing Training Programme’ (LLMC, 2010). There are also examples of much shorter introductory GPN courses of 2–3 days duration available in London provided by a range of independent companies.
Phase 2 testing
Phase 2 (Table 3) of the project is now underway to test and evaluate the effectiveness of the QISS when used by training hubs and other education commissioners in negotiating minimum course requirements to inform consistent HEI curriculum development to be ‘QISS compliant’. The goal is to refine the QISS and embed it as part of the ongoing negotiation between education commissioners and providers, giving nurses and their employers clarity about standardised course content and outcomes. Testing begins in September 2020 in collaboration with HEE, training hubs and the 7 London providers of GPN education.
Table 3. Qualification in Specialism Standard (QISS) Phase 2
| Develop a test-group in the field, involving Health Education England (HEE), education commissioners and providers |
| Test the use of the GPN QISS |
| Refine the QISS and support implementation by training hubs |
Preparatory work for Phase 2 is underway and Capital Nurse is working closely with stakeholders to achieve completion of the project by March 2021.
Discussion
The potential impact of implementing the QISS is significant and could provide a blueprint for GPN education commissioning outside Greater London. It provides an opportunity to bring all HEIs together with a common set of standards producing a unified approach to the curriculum, outcomes, learning support and academic qualifications. This would be a huge step forward for general practice nursing and provides an underpinning foundation for several other related initiatives currently under development. The ‘new to practice’ fellowships would be enhanced by a common coherent programme pathway. The exploration of the Specialist Practice Qualification by the Nursing and Midwifery Council (NMC) (2020) and the discussion about a general community qualification versus a specialist one could be enriched by the identification of what constitutes the education resulting in a competent ‘general’ as opposed to ‘advanced’ or ‘specialist’ nurse in general practice. The review of the HEE career and education framework (HEE, 2015) with updated competences for each level of seniority could benefit from the groundwork already completed with QISS stakeholders. From an optimistic point of view, future potential GP contract negotiations that might examine the need to mandate employment standards for GPNs would be strengthened with an analysis of the benefits of a common core education.
In the evolving primary care architecture, with complex inter-related structures endeavouring to link health and social care delivery to local population needs, it can be easy to forget about some of the key staff groups at the frontline. The PCN contract (NHSE, 2020) has generated a focus on developing new roles in primary care, to support care delivery and sustain general practice, without any apparent connection to the existing valuable resource of GPNs. It is vital that GPNs are properly supported and developed in order to maintain a high standard of first-contact care in general practice. The GPN QISS provides a tool to enable a consistent, accessible and relevant programme of educational preparation for the role, designed by GPNs and experienced colleagues.
Conclusion
The GPN QISS was co-developed in collaboration with a group of stakeholders with a collective expertise on GPN education. The group are convinced there is a place for this set of standards and that it will raise the quality and consistency of education for junior GPNs at a critical point in their career when they need a reliable source of support. As responsibility for education commissioning transfers to regional training hubs with closer connectivity to practice placements and work-based learning, the QISS provides a clear standard to support conversations with HEIs about what should be included in GPN programmes.
There are many GPN 10 Point Plan projects nearing completion that were established to raise the profile of GPNs, making it a first-choice career destination for students and qualified returners to practice, with a clear career pathway supported by sound education and professional support. It will be enlightening to map the outcomes of the GPN 10 Point Plan, including those of the QISS to see how inter-linked and synergistic they are in helping to secure the future GPN workforce.
KEY POINTS
- Some new general practice nurses (GPNs) can feel isolated and have difficulty finding the training they need while learning new skills in the practice
- There are inconsistencies in the content and quality of education programmes that prepare nurses new to general practice for the role
- Capital Nurse engaged with a group of expert stakeholders to co-develop a minimum education standard for GPNs across London
CPD reflective practice
- What are the possible consequences of inconsistent levels of educational preparation for working in general practice?
- What challenges might a nurse new to general practice face when trying to source appropriate training?
- Apart from general practice nurses (GPNs), who else might find the Qualification in Specialism Standard (QISS) valuable?
- What conversations does the QISS facilitate between training hubs and higher education institutions about GPN education?
- What should GP employers know about GPN education?

