The COVID-19 pandemic has radically changed healthcare communication with the requirement of clinicians, nurses, hospital and community staff, and patients, to wear face masks. Health professionals are expected to communicate with patients while maintaining social distancing of 2 metres. Yet, facial expressions are closely tied to our emotions and our faces provide key information of personal identity providing additional information that supports the understanding of speech as well as emotional expression (Carbon, 2020). Wearing masks reduces the ability to access the non-verbal facial expressions and cues, such as lip movements, that are so vital to daily communication. In early June the World Health Organization (WHO) noted that mask use in medical care settings introduces potential harms and risks that ‘should be carefully taken into account’ when caring for members of several populations, including the deaf and hard of hearing community (Chodosh, 2020; WHO, 2020).
Communication
Communication can be defined as transaction and message creation. The process of communication occurs in the context consisting of physical space, cultural and social values, and psychological conditions. Good communication between nurses and patients is essential for the successful outcome of individualised nursing care of each patient (Kourkouta and Papthanasiou, 2014). The Royal College of Nursing (RCN) (2020) recognises that communication is at the heart of everything nurses do. It is central to learning, work and leisure interests. But it is particularly important in health care, where patients/clients feel vulnerable, alone and frightened, and where nurses work alongside colleagues in the health care team who rely on good communication to help them deliver safe, coordinated and effective care. Good communication helps patients feel at ease, feel in control, and feel valued (RCN, 2020 p.24).
Face coverings
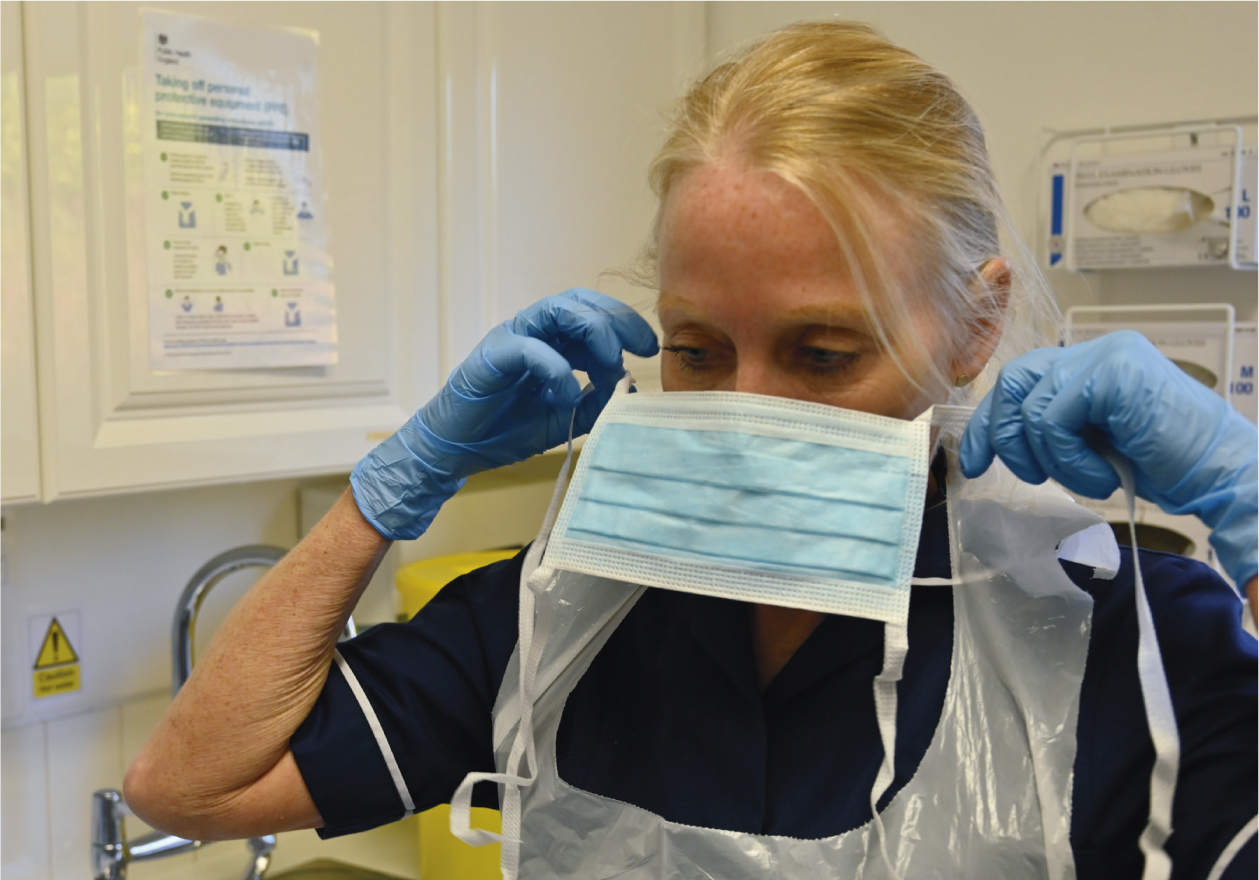
Face coverings are not classified as personal protective equipment (PPE), which is used in a limited number of settings to protect wearers against hazards and risks, such as surgical masks or respirators used in medical and industrial settings. Face coverings are instead largely intended to protect others – not the wearer – from the spread of infection by covering the nose and mouth, the main confirmed sources of transmission of the virus that causes COVID-19.
When it comes to studying faces, the eyes and mouth are the most informative regions because they tend to be the most expressive (Ong, 2020). We subconsciously analyse their combined movements to figure out what someone is trying to tell us. Even so, each feature alone can communicate certain emotions particularly well. The mouth region is good for expressing feelings of happiness. Concealing this area can be problematic when wanting to come across as approachable and friendly (Ong, 2020).
Barriers to communication when wearing face coverings
It is now compulsory to wear face coverings in GP surgeries, hospitals, on public transport and in places where social distancing of 2 metres or more is impossible. However, it is important to recognise that face coverings are not mandatory in all circumstances (Table 1). Compulsory face coverings pose challenges when patients are deaf or have dementia (Carter, 2020). Chodosh et al (2020) recognise that communication between patient and clinician is at the heart of medical care. Even before masks became ubiquitous, people with hearing loss struggled to communicate in healthcare settings, and poor communication was the likely cause of their documented worse health outcomes. Spoken communication has always been challenging in general practice, owing to high levels of noise and poor environmental engineering. Those challenges remain, but masks bring new barriers. In addition to blocking lip movements and facial expressions (which are so important when hearing is marginal), masks muffle the high frequency portions of sound that are essential to speech. Schlögl and Jones (2020) recognise that the COVID-19 pandemic is challenging for older, frail, and cognitively impaired patients. For example, it must be jarring for older people to discuss serious challenges, such as the importance of advance care planning or decisions about do-not-resuscitate orders, with a physician wearing a face mask.
Table 1. Exemptions from face coverings
| Children under the age of 11 (Public Health England does not recommend face coverings for children under the age of 3 for health and safety reasons) |
| People who cannot put on, wear, or remove a face covering because of a physical or mental illness or impairment, or disability |
| Where putting on, wearing, or removing a face covering will cause you severe distress |
| If you are speaking to or aiding someone who relies on lip reading, clear sound or facial expressions to communicate |
| To avoid harm or injury, or the risk of harm or injury, to yourself or others, including if it would negatively impact on your ability to exercise or participate in a strenuous activity |
| Police officers and other emergency workers, given that this may interfere with their ability to serve the public |
Non-verbal communication is inhibited by mask wearing. It is estimated that between 70% and 93% of communication is non-verbal. Practice nurses rely on non-verbal communication as part of a complete holistic assessment and to build therapeutic relationships. The ability to see someone's whole face when communicating allows for a better exchange of information since both speaker and listener can see and interpret body language and facial expressions. We tend to process faces rather than focusing on individual features. If we cannot see the whole face then communicating emotions can be inhibited or lead to misinterpretation of expression or symptoms such as pain. The eyes and mouth are the most expressive features of the face. For those patients who find communication difficult or are hard of hearing, masks can create additional challenges (Chodosh et al, 2020). Sound transition may be quieter more than 2 meters away and it is harder to interpret visual clues when someone has stopped speaking or has paused in speech due to emotion or pain.
Peplau's (1997) interpersonal relations theory suggests that the nurse–patient relationship and therapeutic process requires good communication and involves complex factors such as environment, attitudes, practices and beliefs. Peplau's four phases – orientation, identification, exploitation and resolution – rely on a high level of interpersonal communication between nurses and carers to build trusting, collegiate relationships.
 Practice nurses rely on non-verbal communication as part of a complete holistic assessment and to build therapeutic relationships
Practice nurses rely on non-verbal communication as part of a complete holistic assessment and to build therapeutic relationships
Recommendation for clinical practice to improve communication
There are several things that practice nurses can consider to improve communication:
- Consider face masks with a clear mouth window or face shields
- Make sure that you have the patient's attention before you start talking
- Consider your vocal tone, style, pitch, and rate of your speech
- Talk louder and slower
- Use your hands and your body language
- Demonstrate active listening by using non-verbal messages, summarising, paraphrasing and empathising
- Provide small amounts of information at a time
- Ask the patient if they have understood and allow more time for questions and answers
- If you are talking to a patient for the first time, ask if there is anything you can do to make communication easier for you both
- Try to eliminate any background noises or disturbances whenever possible.
Conclusion
In summary, communication is an essential part of nursing care and practice. Wearing masks can inhibit communication and the therapeutic relationship between patient and practitioners. Additional steps must be taken to remove potential barriers to communication and improve non-verbal communication skills while wearing masks.
KEY POINTS
- Wearing masks reduces the ability to access the non-verbal facial expressions and cues, such as lip movements, that are so vital to daily communication
- When it comes to studying faces, the eyes and mouth are the most informative regions because they tend to be the most expressive
- Additional steps must be taken to remove potential barriers to communication and improve non-verbal communication skills while wearing masks
CPD reflective practice
- What are the main barriers to communication when wearing a mask?
- Which groups of patients are particularly likely to struggle to communicate with masks?
- How could you overcome these barriers?

