Dysfunctional breathing (often termed breathing pattern disorder) is a term that relates to changes in breathing patterns. These are caused by a dysregulation in the feedback loop between the brain and various receptors in the body, changing breathing from an efficient to a less efficient pattern. Dysfunctional breathing can be seen when someone uses the wrong muscles to breathe, uses the upper chest rather than the diaphragm (apical breathing), or breathes through their mouth rather than their nose. Breathing often loses its regular rhythm and may become variable in rate, flow and volume. It reflects a change in the mechanics of breathing and can occur alongside or without a specific lung condition. This change can feel sudden or can build up over time and there are many causes. Depending on the cause, treatment usually consists of a course of breathing pattern retraining from a physiotherapist or in combination with psychologists.
Normal breathing regulation process
The ‘breathing drive’ is responsive to the body's requirements detected by feedforward and feedback loops from the brain and receptors in the respiratory system, with underlying ‘background’ control from the brain stem and autonomic nervous system. Central and peripheral chemoreceptors, as well as mechanoreceptors in the lungs, convey sensory and neural input to the brain to help modulate respiratory drive (Brinkman et al, 2021):
- Peripheral chemoreceptors detecting changes in the levels of oxygen and carbon dioxide – located in the arterial aortic bodies and the carotid bodies
- Central chemoreceptors that are primarily sensitive to changes in the pH in the blood, resulting from changes in the levels of carbon dioxide – located on the medulla oblongata
- This is then compared with afferent or conducting information on actual ventilation from a number of sources including (Sharma et al, 2015):
- Pulmonary stretch receptors
- Chest wall and skin receptors
- Pulmonary C nerve fibres and
- Skeletal muscle ergo-receptors (nerve fibres that are sensitive to metabolites).
For example, during exercise oxygen consumption rises and so does the production of carbon dioxide. Without alteration to the respiratory rate, anaerobic respiration results, as does the acidity of the blood, caused by the accumulation of carbon dioxide. The respiratory centre in the medulla and pons responds by altering its firing pattern to change breathing rhythm and volume (Brinkman et al, 2021).
Dysfunctional breathing
When the interpretation of information from this feedforward/feedback loop from the brain and the receptors is mismatched, this can give rise to inappropriate responses in how someone breathes to harmless stimuli. For example, someone could experience an excessive perception of breathlessness to mild exertion or over-breathe from stress triggers.
Dysfunctional breathing is well recognised to occur in people presenting with excessive or disproportionate breathlessness, both in those with or without long-term lung conditions (Barker and Everard, 2015). It also occurs alongside obesity, neuromuscular disease and with drug administration causing respiratory depression (Brinkman et al, 2021). Hyperventilation, for example, (which is one presentation of disordered breathing) can trigger asthma through excessive volumes of air taken in through mouth breathing (Meuret and Ritz, 2010). With progressive chronic obstructive pulmonary disease (COPD), where air trapping (inability to fully exhale) occurs, some patients tend to take shallow, apical breaths using accessory muscles rather than more efficient abdominal breaths. Box 1 explores the typology of dysfunctional breathing.
Box 1.TypologyThere is no formal definition of dysfunctional breathing and the term has referred in the past to a group of breathing disorders. In more recent years, researchers have sought to identify different types of dysfunctional breathing.Hyperventilation is a normal reaction to stressful stimuli, after which breathing should return to normal. When we breathe more than the body needs this can cause a chemical imbalance (alkalosis) due to a lowering of carbon dioxide (hypocapnia). But if there is a prolonged stress or repeated exposure to a trigger, the body can start to get used to this altered inefficient pattern without the person realising. This can lead to people experiencing unpleasant symptoms, including breathlessness, which is disproportionate to activity or disease, or sensations related to hyperventilation such as tinglingExercise-induced hyperventilation occurs in a subgroup of these patients and applies to those who develop chest discomfort and dyspnoea without bronchospasm and that is unresponsive to beta agonistsPostural hyperventilation can occur when the patient moves from lying to standing, thought to be due to changes in the vestibular system affecting the autonomic nervous systemPeriodic deep sighing, up to 15 times in a 15-minute period, with associated dyspnoeaVocal cord dysfunction (VCD), where there is abnormal and excessive closure of the vocal folds, typically during inspiration, is a well-defined and distinct disorder, where the source is extra-thoracic and treated via ENT and speech therapy. It is sometimes confused with asthma, but the difference is that the vocal cords tighten, not the airways. To add to the confusion, many people with asthma also have VCDThoracic dominant breathing or apical breathing, with little lateral or abdominal breathing, often due to respiratory or cardiac disease or in obesityForced abdominal expiration, with excessive and inappropriate contraction of the abdominals. This may be a normal adaptation in those with COPD, but is considered dysfunctional otherwiseThoraco-abdominal asynchrony or paradoxical breathing, where there is asynchrony between the rib cage and the abdomen, resulting in ineffective breathing. This is a normal response to upper airway obstruction, acute respiratory failure and neuromuscular disorders but is considered dysfunctional otherwiseBoulding et al, 2016; American Academy of Allergy, Asthma and Immunology, 2021
Common triggers
Common triggers for dysfunctional breathing include:
- Anxiety or stress
- Acute illness, eg chest infection, pneumonia
- Long-term respiratory condition, eg COPD, asthma
- Post-viral
- Hormonal changes at puberty or menopause
- Traumatic event – physical or emotional.
Aggravating factors
Aggravating factors for dysfunctional breathing include:
- Pain – especially in the abdomen or lower back
- Digestive issues, eg reflux, hiatus hernia.
Signs
As dysfunctional breathing is relatively common and can be easily missed, the role of the GPN is to consider it as a potential cause of unexplained breathlessness. The signs may be:
- Mouth breathing
- Increased tidal volume or respiratory rate. This desire to take bigger breaths is often described as ‘air hunger’
- Apical breathing rather than diaphragmatic breathing
- A higher ratio of inspiratory to expiratory length
- Excessive yawning or sighing
- A lack of pause between expiration and inspiration.
Symptoms
Symptoms of dysfunctional breathing include:
- Respiratory alkalosis caused by a fall in blood carbon dioxide due to hyperventilation/panic leading to: fainting, tingling, tetany and numbness
- A feeling of not being able to take a deep breath or an unsatisfied breath in
- Light headedness/dizziness
- Feeling bloated
- Aching and tightness in the muscles around the jaw, neck and shoulders
- Feeling permanently exhausted and unable to concentrate for no apparent reason
- Dry cough or constant throat clearing
- Chest or throat discomfort
- Excessive breathlessness in relation to activity.
Diagnosis
There is no gold standard diagnostic assessment tool and instead Courtney et al (2011) suggests a multi-component assessment including:
- Use of a valid questionnaire
- Breathing pattern evaluation
- Biochemical assessment, particularly carbon dioxide measurements.
The Nijmegan Questionnaire (van Doorn et al, 1982) (see Table 1), for example, is a commonly used instrument, developed to screen for hyperventilation syndrome, which represents only one type of dysfunctional breathing. This may lead to the under-recognition of dysfunctional breathing, or symptoms may be wrongly attributed to other causes – however, it has been shown to be a good symptom indicator and responsive to change after breathing pattern retraining. It is an easy tool to use in a clinic setting to help build a picture of breathing-related symptoms.
Table 1. The Nijmegen questionnaire
| The patient circles the number in the column that best represents what they have felt recently* | |||||
|---|---|---|---|---|---|
| Never | Rarely | Sometimes | Often | Very often | |
| Chest pain | 0 | 1 | 2 | 3 | 4 |
| Feeling tense | 0 | 1 | 2 | 3 | 4 |
| Blurred vision | 0 | 1 | 2 | 3 | 4 |
| Dizzy spells | 0 | 1 | 2 | 3 | 4 |
| Feeling confused | 0 | 1 | 2 | 3 | 4 |
| Faster or deeper breathing | 0 | 1 | 2 | 3 | 4 |
| Short of breath | 0 | 1 | 2 | 3 | 4 |
| Tight feelings in the chest | 0 | 1 | 2 | 3 | 4 |
| Bloated feeling in the stomach | 0 | 1 | 2 | 3 | 4 |
| Tingling fingers | 0 | 1 | 2 | 3 | 4 |
| Unable to breathe deeply | 0 | 1 | 2 | 3 | 4 |
| Stiff fingers or arms | 0 | 1 | 2 | 3 | 4 |
| Tight feelings round mouth | 0 | 1 | 2 | 3 | 4 |
| Cold hands or feet | 0 | 1 | 2 | 3 | 4 |
| Palpitations | 0 | 1 | 2 | 3 | 4 |
| Feelings of anxiety | 0 | 1 | 2 | 3 | 4 |
| Subtotals | |||||
| Total | |||||
Diagnosis relies also on the exclusion of organic disease, careful history taking and objective examination of the breathing pattern both at rest and on exertion. The general practitioner or advanced practitioner needs to undertake a differential diagnosis (Baxter and Lonergan, 2020).
For nurses managing long-term respiratory conditions in primary care, there is an obvious need to consider whether dysfunctional breathing is present alongside lung disease or whether the symptoms are due to suboptimal condition management. If the latter is suspected the nurse will aim to maximise self-care.
Prevalence
Estimates of prevalence of dysfunctional breathing vary, due to the difficulties in screening:
- Hyperventilation in children and teenagers can vary from 18.6% in those without asthma to 55% for those with asthma (Gridina et al, 2013)
- Breathing pattern disorders in children with asthma range in the literature from 5.3% (de Groot et al, 2013) to 35% (Hepworth et al, 2019)
- In adults it varies less, with the literature showing prevalence ranging from 29–36% (Thomas et al, 2001; Connett and Thomas, 2018).
Management of dysfunctional breathing in primary care
An accurate diagnosis and explanation can provide reassurance and relief of anxiety, which may in itself reduce symptoms. Breath retraining is the most common form of management. The availability of different types of breath retraining from local physiotherapy teams varies. Management includes:
- The Buteyko technique: a breathing re-education programme focusing on efficient nasal breathing and controlled pauses with the aim of reducing hyperventilation over time. This training is available to all allied health care practitioners, nurses, doctors and physiotherapists
- The Papworth method: a sequence of integrated breathing and relaxation exercises that ameliorates respiratory symptoms, dysfunctional breathing and adverse mood compared with usual care (Holloway and West, 2007)
- Yoga classes for people with COPD and asthma have been trialled, but not enough evidence yet exists (Boulding et al, 2016)
- Sinus rinsing to allow nose breathing to be normalised
- Since the psyche plays a role in nearly all respiratory problems, a referral to a psychologist may be necessary, particularly in chronic disease or where there may be an indication of underlying psychogenic causes (Niggemann et al, 2017)
- Box 2 and Figure 1 provide some simple exercises that GPNs can recommend for patients with dysfunctional breathing.
Box 2.Simple exercises and changes that GPNs could recommendNose-breathingEncourage the patient to close their mouth and breathe through their nose. For some with dysfunctional breathing, this will feel strange, but the brain will learn this new pattern. The nose warms, cleans and filters the air and encourages diaphragmatic breathingTriggersUnderstanding and managing triggers such as anxiety, acid reflux or painDiaphragmatic breathing (tummy breathing)Invite the patient to sit in an upright or inclined position with the back well supported. Invite them to place one hand on the upper chest and one on the tummy. Encourage steady and relaxed breaths rather than large breaths. Focus on them moving the tummy rather than the chest when they breathe. They should feel the hand on the tummy rise and fall as they breatheBox breathing (Figure 1)This technique helps patients to regulate their breathing pattern and encourages longer expiration compared to inspiration. It also helps distract from breathlessness and anxiety
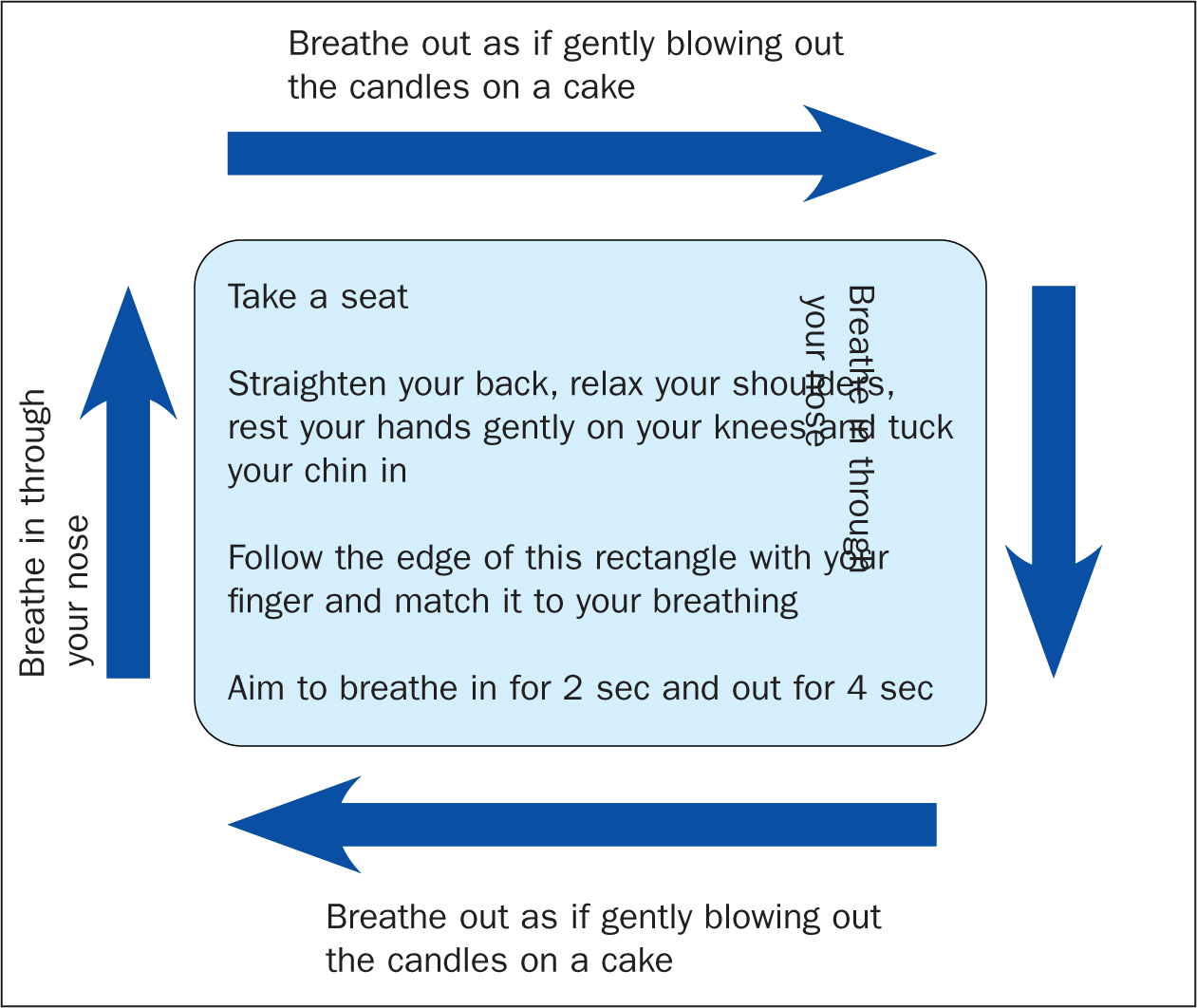 Figure 1. Box breathing exercise
Figure 1. Box breathing exercise
Summary
Respiration is a complex process that relies on co-ordination of the body between the muscles of respiration and the control centre in the brain. Often in response to a trigger or disease, breathing patterns can change and can become fixed. This leads to a range of symptoms that can be confused with respiratory and cardiac disease. Currently there are few reliable diagnostic tests, meaning that the nurse must be alert to the possibility of dysfunctional breathing, which may be responsive to breath retraining.
Useful resources:
- Physiotherapy in the management of children with asthma and altered breathing patterns. Royal Brompton & Harefield hospitals. https://www.rbht.nhs.uk/our-services/paediatrics/paediatric-rehabilitation-and-therapies/paediatric-physiotherapy/physiotherapy-management-children-asthma-and-altered-breathing-patterns
- Physiotherapy in the management of children with asthma and altered breathing patterns - resources. Royal Brompton & Harefield hospitals. https://www.rbht.nhs.uk/our-services/paediatrics/paediatric-rehabilitation-and-therapies/paediatric-physiotherapy/physiotherapy-management-children-asthma-and-altered-breathing-patterns/physiotherapy-management-children-asthma-and-altered-breathing-patterns-resources
- Physiotherapy in the management of teenagers and young adults with asthma and altered breathing patterns. Royal Brompton & Harefield hospitals. https://www.rbht.nhs.uk/our-services/paediatrics/paediatric-rehabilitation-and-therapies/paediatric-physiotherapy/physiotherapy-management-teenagers-and-young-adults-asthma-and-altered-breathing-patterns
- Physiotherapy in the management of teenagers and young adults with asthma and altered breathing patterns - resources. Royal Brompton & Harefield hospitals. https://www.rbht.nhs.uk/our-services/paediatrics/paediatric-rehabilitation-and-therapies/paediatric-physiotherapy/physiotherapy-management-teenagers-and-young-adults-asthma-and-altered-breathing-patterns/physiotherapy-management-teenagers-and-young-adults-asthma-and-altered
- Baxter N, Lonergan T. The differential diagnosis of the breathless patient. Primary Care Respiratory Update. 2020. https://www.pcrs-uk.org/sites/pcrs-uk.org/files/WW%20-%20Breathlessness%20PROOF%202.pdf
- Physiotherapy for breathing pattern disorders. https://www.physiotherapyforbpd.org.uk/
- Sonnappa S, Wells C. (2015) Breathing Pattern Disorders. In: European Respiratory Society. Handbook of Respiratory Medicine. Chapter 15. 732–738
KEY POINTS:
- General practice nurses (GPNs) may identify unexplained respiratory symptoms such as breathlessness and cough. In such cases, they should look for the signs and symptoms of dysfunctional breathing patterns
- It is essential that underlying pathology is ruled out, and dysfunctional breathing is identified and treated, as it is closely related to higher anxiety, poorer quality-of-life and higher levels of morbidity for both adults and children
- Dysfunctional breathing may or may not occur alongside a range of respiratory, cardiac or neurological diseases
- Assessment includes screening questionnaires, breathing pattern evaluation and biochemical screening, particularly for respiratory alkalosis caused by a fall in blood carbon dioxide
- Once a diagnosis is made, treatment usually involves breathing pattern retraining
CPD reflective practice:
- Having read this article, what one change would you make to your clinical practice?
- Spend the next week observing for the signs and symptoms of breathing dysfunction in people who are breathless. What happened? What did you learn?
- Find a way to share to share your learning with peers: this may be a conversation or more formally with your immediate team, GPN group or primary care network


