At the end of each year, the Global Initiative for Obstructive Lung Disease (GOLD) publishes its guidance on chronic obstructive pulmonary disease (COPD) for the following year. The latest recommendations for 2023 will have an impact on how we manage people with COPD, with an important change being made regarding treatment options (GOLD, 2022). This affects general practice nurses (GPNs) who support people living with COPD, whether they are prescribers or not, as a COPD review should include consideration of the individual's characteristics, symptoms, risk of exacerbations and personal preferences, all of which will affect treatment decisions. GPNs should be acting as the patient's advocate, supporting them with shared decision-making to plan their care in the most effective way. This article offers a summary of:
- The updated definition of COPD and the recommended approach to diagnosis
- The place for computerised tomography (CT) scanning in COPD
- Pharmacological and non-pharmacological treatment options
- The appropriate use of inhaler devices
- Tailoring inhaled therapies: from ABCD to ABE
- Exacerbations and comorbidities.
The focus will be on the role of primary care in diagnosing and managing COPD, including how to recognise when patients need referring on to specialist services. The article references the new guidelines, but detailed information about the evidence that informs them can be found by accessing the specific pages, tables and figures mentioned throughout.
Diagnosing and defining COPD
An updated definition of COPD is included in the guidelines, reflecting the symptoms (productive cough and breathlessness) that are linked to persistent, often progressive and non-fully reversible airflow obstruction. These are caused by pathophysiological changes in the airways and/or alveoli. The guidelines reinforce the concept of two key ‘types’ of COPD: chronic bronchitis and emphysema (GOLD, 2022: p5). Chronic bronchitis is defined by the presence of chronic cough and sputum for at least 3 months a year for at least 2 years, and where no other cause is evident (GOLD, 2022: p13). GOLD reports that up to 35% of people with COPD will have chronic bronchitis. The diagnosis is based on symptoms, risk factors and spirometry findings but also by recognising which symptoms are most significant for each individual.
The place for computerised tomography scans in people with COPD
Computerised tomography (CT) scans offer more information than a chest X-ray and can be helpful when trying to ascertain the cause of symptoms such as excessive sputum production, which might be due to coexisting bronchiectasis (Huang et al, 2022). GOLD recommends CT scans for people with COPD who are having recurrent exacerbations, people with significant hyperinflation and an FEV1 <45% predicted, those with symptoms which are at odds with the level of lung function impairment (although there is a known disparity between these two) and also for people who meet the criteria for lung cancer screening (GOLD, 2022: p43). In secondary or tertiary care, CT scanning may also help to identify people who could benefit from endobronchial valve therapy or lung volume reduction surgery (GOLD, 2022: p44).
‘The ABE approach underlines the significant impact that exacerbations can have in the management of COPD, independent of the symptom burden.’
Treatment options for COPD
The main aims when treating COPD are to reduce morbidity, exacerbations and mortality. Previous trials have failed to demonstrate convincing evidence that drugs used to treat COPD reduce mortality, but GOLD has recognised that two recent studies, IMPACT (Lipson et al, 2018) and ETHOS (Rabe et al, 2020), have now shown an impact on all-cause mortality when using triple therapy – an inhaled corticosteroid, a long-acting beta2 agonist and a long-acting muscarinic antagonist in a triple therapy inhaler – when compared to a dual bronchodilator (GOLD, 2022: p67). GOLD has put together a table which links to the evidence from randomised controlled trials, and which supports the use of pharmacotherapy (such as dual bronchodilator or triple therapy) and non-pharmacological interventions (smoking cessation, pulmonary rehabilitation, lung volume reduction surgery, non-invasive positive pressure ventilation and long-term oxygen therapy) to reduce mortality in different groups of people living with COPD. These updated recommendations act as an important reminder for primary care clinicians to implement interventions that are relevant in the community setting and to refer on for more specialised interventions in secondary care as appropriate (GOLD, 2022: p68).
Device choice, inhaler technique and adherence
Irrespective of whether people living with COPD need a dual bronchodilator or triple therapy (and it could be argued that these are the two key therapies to consider when treating COPD in the future), nothing will work unless it is taken regularly and correctly. Inhaler technique needs to be taught and assessed, visually and/or with an objective inspiratory flow rate measure. Clinicians can use the ADMIT and Asthma + Lung UK websites for more information about inhaler devices and technique; these resources can also be shared with patients and carers. GOLD recognises the potential for using smart inhalers in the future, as evidence suggests that these can provide objective information about technique and adherence (Bowler et al, 2019). The environmental impact of different inhalers is highlighted, and clinicians in the UK will be working with recommendations from the Impact and Investment Fund (IIF) to address this (NHS England, 2022). However, the right inhaler depends on the individual who is using it and discussions as to which inhaler device is most appropriate should involve a shared decision-making approach. GOLD reminds clinicians that the choice of whether to use pressurised metered dose inhalers (pMDIs), with or without spacers, or soft mist or dry powder inhalers, should only be made after a full and tailored assessment (GOLD, 2022: p69; p112).
The section on adherence is important, as it highlights research that shows 22–93% of people living with COPD fail to take their medication as prescribed, even in severe disease (GOLD, 2022: p71). Clinicians may increase adherence by reducing the number of inhalers used and the limiting the type of devices to the same type where possible. This again suggests that dual bronchodilators and triple therapy may have benefits in terms of how they combine key drugs that impact outcomes in one device.
Optimising the management of COPD: from ABCD to ABE
One of the most recognisable elements of the GOLD guidance in recent years has been the ABCD assessment tool, where recommendations regarding treatment classes were made based on the individual's symptom burden and their risk of exacerbations, the latter being based on their previous history of exacerbations. However, the new update has dispensed with the ABCD algorithm and replaced it with the ABE assessment tool. The ABE approach underlines the significant impact that exacerbations can have in the management of COPD, independent of the symptom burden (GOLD, 2022: p115) (Figure 1). Classes A and B reflect symptom scores based on the modified Medical Research Council (mMRC) dyspnoea score and/or the COPD assessment test (CAT) score, as in previous versions of GOLD. However, the E category, which replaces C and D, reflects the importance of recognising that people who have had two or more exacerbations, or one exacerbation that has required hospital admission, are high risk for future exacerbations and need to be treated with this in mind, irrespective of their mMRC or CAT scores.
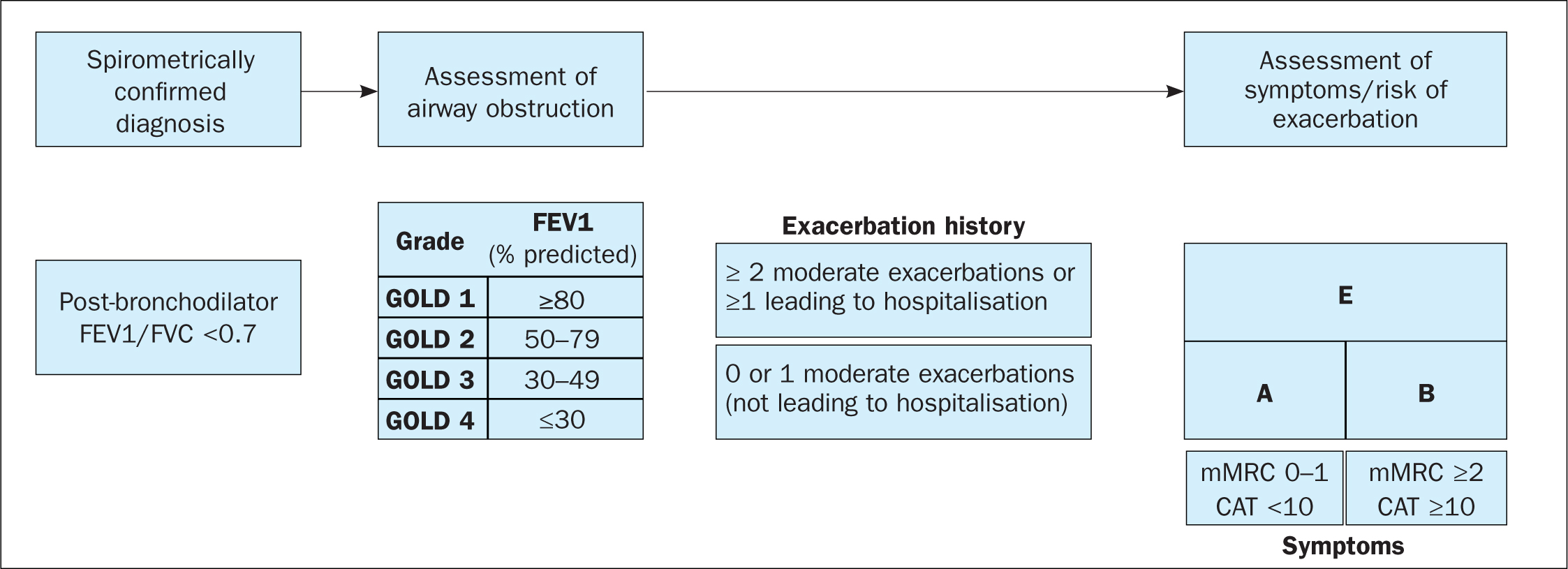
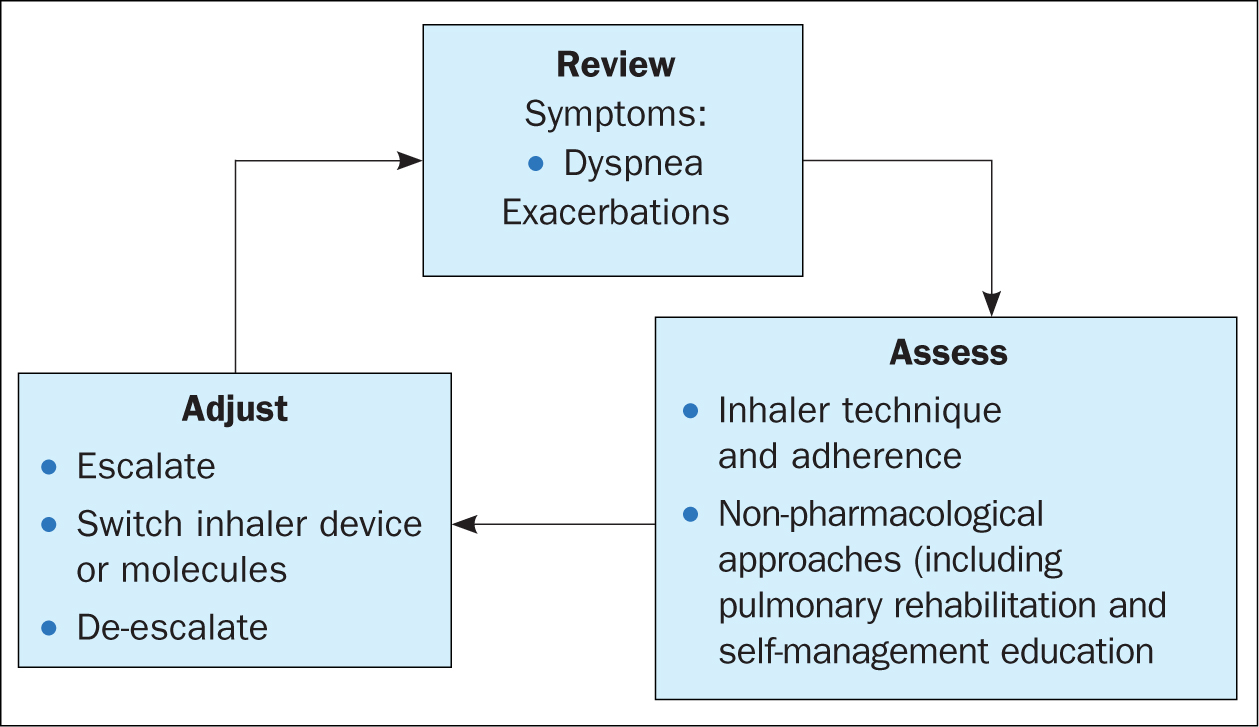
The ABE assessment tool is used for the initiation of inhaled therapy and recommends that any bronchodilator can be used for category A (low symptom burden, low risk of exacerbations), although a long-acting version may be preferable. A dual bronchodilator is recommended for category B (higher symptom burden but still low risk of exacerbations), with dual bronchodilators or triple therapy for category E. It is interesting to compare this approach to that published by the National Institute for Health and Care Excellence (NICE, 2018), which recommends a single short-acting bronchodilator, a dual bronchodilator or triple therapy based on symptoms and/or exacerbations. NICE (2018) recommends combinations of inhaled corticosteroids with long-acting beta2 agonists in people where there is evidence of reversibility (ie, where there is a history of asthma with fixed airways disease), but GOLD 2022 does not include a recommendation for ICS/LABAs (GOLD, 2022: p115). The ‘assess, adjust, review’ approach from previous publications is reiterated (Figure 2), with escalation of treatments based on whether the main presenting feature is breathlessness or exacerbations (GOLD, 2022).
Exacerbations and comorbidities
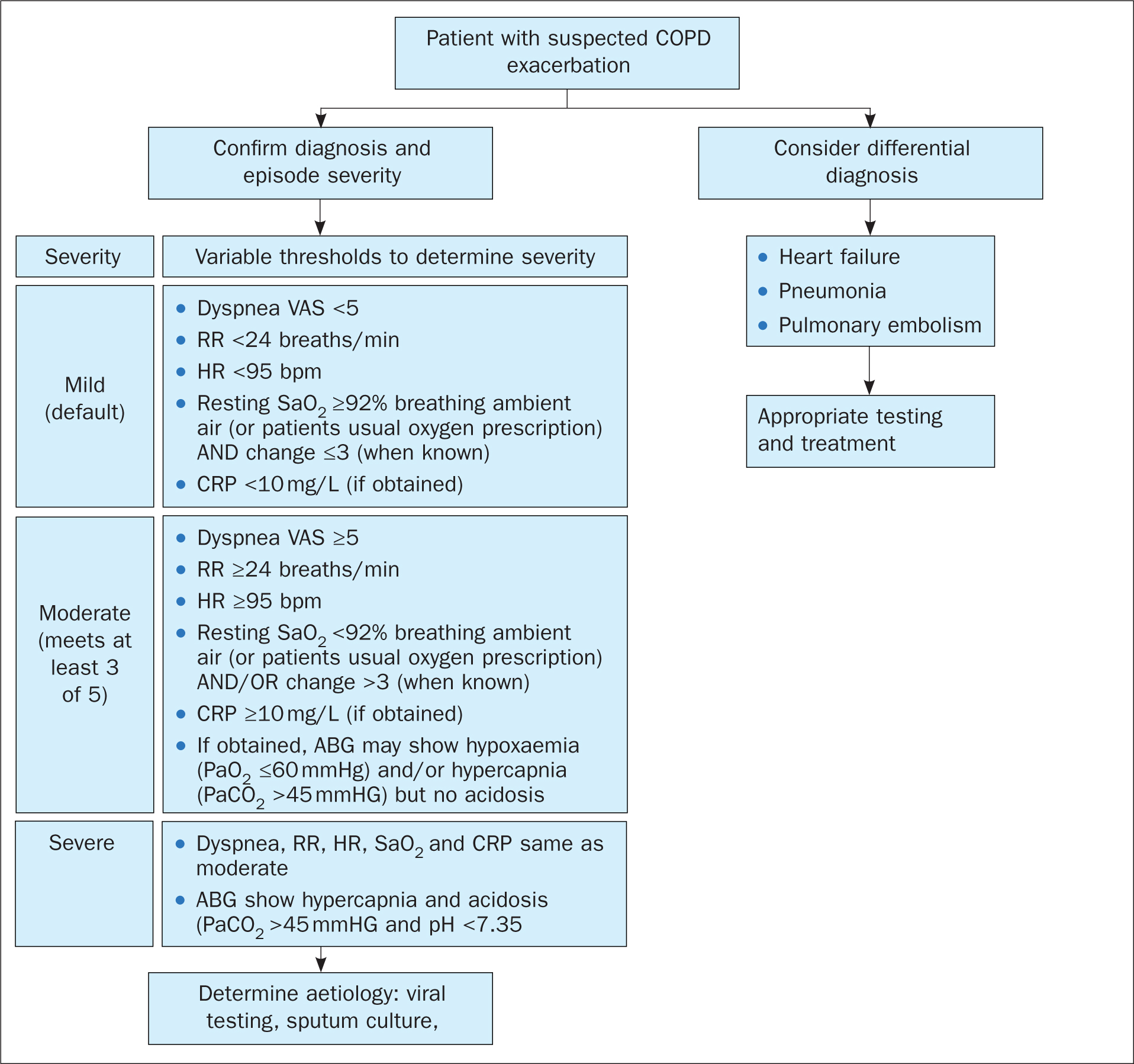
The updated sections on exacerbations remind clinicians of the importance of considering comorbid or new diagnoses as the cause of any symptoms. Specific diagnoses to be considered include:
- Pneumonia
- Pulmonary embolism
- Pneumothorax
- Pleural effusion
- Cardiac conditions, such as heart failure, atrial fibrillation or myocardial infarction.
Exacerbations are described as acute events, occurring over a period of less than 14 days, where usual symptoms such as breathlessness, cough and sputum production increase, often accompanied by tachypnoea and tachycardia. GOLD describes the drivers of these symptoms as local and systemic inflammation, caused by infection, pollution or other insults to the airways (GOLD, 2022: p134). Anyone presenting with a suspected exacerbation should have a full assessment to determine possible causes, the severity of any COPD exacerbation and immediate and ongoing management.
Figure 3 summarises the key elements that will enable a clinician to establish the severity of the exacerbation and whether the patient will require admission to hospital. The recommended approach to assessment in primary care includes measuring heart and respiratory rate and oxygen saturations, and asking the patient to score their dyspnoea using a visual analogue scale (VAS). Blood C-reatrive protein (CRP) levels can also be used if available (GOLD, 2022: p136). GOLD recognises that more than 80% of exacerbations of COPD are managed in the primary care setting and that management will be based on optimising the use of inhaled therapies, particularly bronchodilators, with the addition of antibiotics and/or oral corticosteroids where indicated (GOLD, 2022: p140).
Conclusion
GOLD regularly reviews its guidance on the definition, diagnosis and management of COPD based on new research findings and publishes updated recommendations annually. The 2022 guidance, which supports practice for 2023, has reviewed all these areas. GPNs are often involved in the diagnosis and management of COPD and should be aware of this update and consider how it impacts on their role. One of the most important changes to this guidance is the move from the ABCD assessment tool to the new ABE approach. This reflects a renewed focus on the importance of reducing the risk and impact of acute exacerbations of COPD. The potential for triple therapy to reduce all-cause mortality in particular patients is also highlighted in this update (GOLD, 2022).
KEY POINTS:
- General practice nurses are often involved in the diagnosis and management of chronic obstructive pulmonary disease (COPD) and should be aware of the GOLD update and consider how it impacts on their role
- Diagnosis is based on symptoms, risk factors and spirometry findings but also by recognising which symptoms are most significant for each individual
- The right inhaler depends on the individual who is using it and discussions as to which inhaler device is most appropriate should involve a shared decision-making approach
- The new ABE assessment tool reflects a renewed focus on the importance of reducing the risk and the impact of acute exacerbations of COPD
CPD REFLECTIVE PRACTICE:
- How often do you assess inhaler technique in your chronic obstructive pulmonary disease patients? Why is this important?
- What are the key things to consider in a patient presenting with an exacerbation?
- How will this article change your clinical practice?


