This material has been created and fully funded by Alliance Pharmaceuticals and is for UK Healthcare Professionals only.
Prescribing information and adverse event reporting details can be found at the end of this document.
The burden of malnutrition
Malnutrition affects over 3 million people in the UK and is a major health and economic problem, costing the UK health and social care system more than £23 billion each year.1-3 In the primary care setting, malnutrition is a common yet under-recognised condition which affects up to 11% of patients visiting their GP in the UK.4
When left untreated, malnutrition can lengthen hospitalisation, reduce quality of life and increase the risk of developing other diseases.5
In comparison to healthy individuals, malnourished patients may also be associated with a wide range of physical and clinical consequences, including:4
- Higher mortality
- Reduced muscle strength and frailty
- Slower recovery from illness and surgery
- Impaired wound healing
- Compromised immune response
To help reduce malnutrition, identifying and screening people at risk of malnutrition can be carried out within primary care. In fact, tackling malnutrition can improve clinical outcomes, reduce health care use and costs.4
NICE quality standard (QS24) highlights:6
- The need for all care services to take responsibility for the identification of people at risk of malnutrition
- To provide nutritional support for those who need it
- To take an integrated approach to the provision of services
Identifying at-risk patients in primary care
Some initial signs and symptoms of malnutrition to look out for amongst patients in primary care can include unintended weight loss or appearing thin, fragile skin, recurrent infections, feeling tired or cold, and a lack of appetite.4Reviewing patient medical history i.e. weight, medication, and prior surgery, alongside asking the appropriate questions during patient discussion, are important first steps in the identification of malnourished patients.
Key questions that can help identify malnutrition in patients could include:4
- How is your appetite lately? How are you managing with your eating and drinking?
- Have you recently changed what/how often you're eating?
- How would you describe your weight? What is a usual weight for you?
- How does food taste? Do you enjoy eating?
- Do you feel like your weight has changed in the last few weeks or months?
- How are your clothes and jewellery fitting? Do they feel like they fit differently than usual?

Patients that may be at risk of malnutrition include those with medical conditions such as:7 - 8
- Long term illnesses/disease (e.g. diabetes, and kidney disease)
- Chronic progressive conditions (e.g. cancer or dementia)
- Digestive/malabsorption conditions, such as Crohn’s disease
- Receiving treatment or recovering from surgery
- Mental health conditions
- Drug or alcohol dependency
Screening
You can help identify patients who may be at risk of malnutrition by using a widely used screening tool such as the Malnutrition Universal Screening Tool (MUST).9 - 10 Visit the MUST tool on the BAPEN website here for more information.
Management and Guidelines
In many cases, malnutrition can be managed using dietary advice and treatment goals to optimise food intake.4 Dietary advice includes:11
- Encouraging small, frequent meals and snacks
- Choosing full fat and sugar products rather than ‘low fat and sugar’
- Enriching the diet with energy and protein
- Including nutrient-rich drinks
Oral nutritional supplements (ONS) can be used when food intake has been insufficient, or when it is anticipated that food alone will not meet nutritional requirements.4
If there is a concern about the adequacy of micronutrient intake:
- NICE Clinical Guidelines 32 recommends that oral multivitamin and mineral supplements should help individuals who are eating poorly to meet their vitamin and mineral requirements.9
- NHS England has advised Integrated care boards (ICBs) that for people with medically diagnosed deficiencies or who have undergone surgery that results in malabsorption, vitamins and minerals can be prescribed in primary care.12
- BOMSS Guidelines for patients undergoing bariatric surgery recommend FORCEVAL® Capsules as a suitable multivitamin supplement following a range of bariatric surgery options.13
Choose a comprehensive, licensed multivitamin
Not all supplements provide patients with a comprehensive vitamin and mineral formulation.
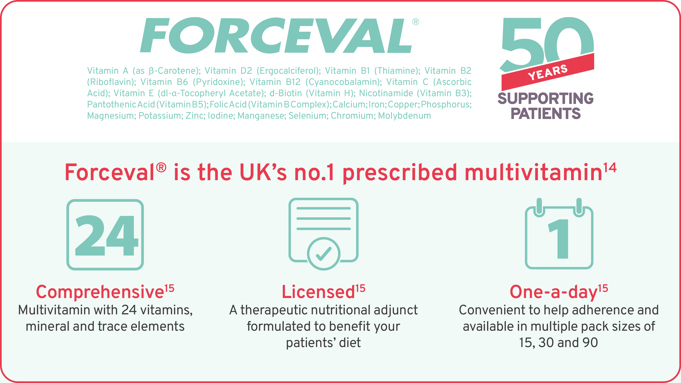
Forceval® Capsules is the no. 1 prescribed multivitamin in the UK.14
Comprehensive15
Multivitamin with 24 vitamins, mineral and trace elements.
Licensed15
A therapeutic nutritional adjunct formulated to benefit your patients’ diet.
One-a-day15
Convenient to help patient adherence and available in multiple pack sizes of 15, 30 and 90.
FORCEVAL® Capsules can be used as a therapeutic nutritional adjunct for patients who are 12 years old and above and have been medically diagnosed with vitamin and mineral deficiencies due to factors such as illness, lifestyle, or chronic conditions that put them at risk of malnutrition.15
Recommend FORCEVAL® Capsules, a licensed formulation with over 50 years of experience,16 helping you to support the management of malnourished patients.
Click here for more information and to go to Forceval.co.uk (promotional website).
Please consult the Summary of Product Characteristics for a full listing of contra-indications, precautions, and adverse events before prescribing this medicine. Rash, nausea, vomiting and abdominal pain have been reported. Should not be given to individuals with known allergies to peanut or soya.
NICE; National Institute of Health and Care Excellence, BAPEN; British Association for Parenteral and Enteral Nutrition, BOMSS; British Obesity & Metabolic Surgery Society.
PRESCRIBING INFORMATION for Forceval® Capsules
Presentation: Brown and maroon, oblong, soft gelatin capsule printed containing: Vitamin A (as β-Carotene) 2,500.0 iu; Vitamin D2 (Ergocalciferol) 400.0 iu; Vitamin B1 (Thiamine) 1.2 mg; Vitamin B2 (Riboflavin) 1.6 mg; Vitamin B6 (Pyridoxine) 2.0 mg; Vitamin B12 (Cyanocobalamin) 3.0 mcg; Vitamin C (Ascorbic Acid) 60 mg; Vitamin E (dl-α-Tocopheryl Acetate)10 mg; d-Biotin (Vitamin H) 100 mcg; Nicotinamide (Vitamin B3) 18 mg; Pantothenic Acid (Vitamin B5) 4.0 mg; Folic Acid (Vitamin B Complex) 400 mcg; Calcium 108 mg; Iron 12 mg; Copper 2.0 mg; Phosphorus 83 mg; Magnesium 30 mg; Potassium 4.0 mg; Zinc 15 mg; Iodine 140 mcg; Manganese 3.0 mg; Selenium 50 mcg; Chromium 200 mcg; Molybdenum 250 mcg.
Indications: As a therapeutic nutritional adjunct in conditions where the intake or absorption of vitamins and minerals is suboptimal, in convalescence from illness or surgery or for patients on special or restricted diets, where food intolerances exist or as an adjunct in synthetic diets.
Dosage: Adults and the elderly: One capsule daily swallowed whole with water, preferably one hour after a meal. Not recommended in children under 12 years of age.
Contra-indications: Hypercalcaemia, haemochromatosis and other iron storage disorders. Hypersensitivity to the active substance(s) or to any of the excipients. Allergy to peanuts or soya.
Precautions: Protein and energy are also required to provide complete nutrition in the daily diet. No other vitamins, minerals or supplements with or without vitamin A should be taken with this preparation except under medical supervision. Do not take on an empty stomach. Do not exceed the stated dose. Contains iron, keep out of the reach and sight of children as overdose may be fatal. Contains E123 (amaranth) and E124 (ponceau 4R red), which may cause allergic reactions. High dose of β-carotene (20-30 mg/day) may increase the risk of lung cancer in current smokers and those previously exposed to asbestos. Patients with thyroid disorders should seek medical advice before taking Forceval Capsules.
Interactions: Folic acid can reduce the plasma concentration of phenytoin. Oral iron and zinc reduce the absorption of tetracyclines.
Side Effects: Hypersensitivity reaction (such as rash) and gastrointestinal disturbances (such as nausea, vomiting and abdominal pain).
Legal Category: P.
Packs and NHS price: 15 capsules (£5.46), 30 capsules (£9.92) or 90 capsules (£28.77).
Marketing Authorisation number: Forceval Capsules PL16853/0079.
Full prescribing information is available from:
Alliance Pharmaceuticals Ltd
Avonbridge House
Bath Road
Chippenham
Wiltshire
SN15 2BB
www.alliancepharma.co.uk
Date of preparation/last revised: April 2022
|
Adverse Event Reporting Adverse events should be reported. Reporting forms and information can be found at https://yellowcard.mhra.gov.uk Adverse events should also be reported to Pharmacovigilance at Alliance Pharmaceuticals Ltd, tel: 01249 466966, email: pharmacovigilance@alliancepharma.co.uk |
JB-002709. January 2024.

